Primary determining factors to be considered for the osseointegration of a dental implant
Oral implantology has revolutionised clinical practice in dentistry by demonstrating that the oral rehabilitation of patients with single, multiple or total tooth loss with dental implants is a predictable treatment with a high success rate. In this sense, the favourable long-term results of oral implant treatment are related to the development of the phenomenon of osseointegration and a good reaction of the peri-implant tissues.
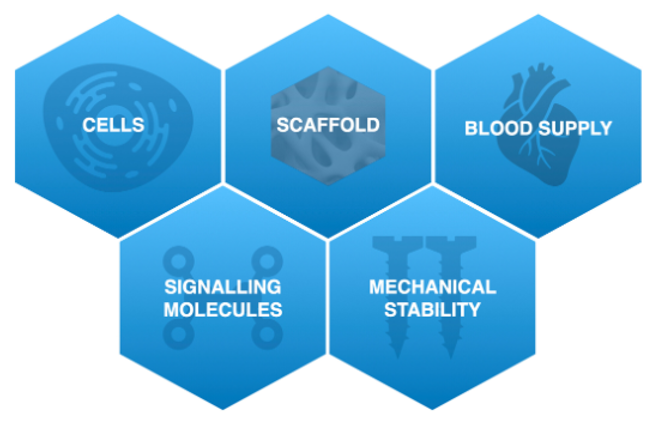
Several key factors are necessary for bone regeneration and eventual osseointegration of a dental implant to occur: cells, clot and blood supply, as well as mechanical stability. However, even when these principles are met, the total amount of regenerated bone, its stability over time and the incidence of complications can vary significantly.

*Microscopic histological section of bone embedded in the titanium surface of a dental implant (black)
Although implant longevity is nowadays considered highly accurate, continuous efforts are made to fine-tune the long-term success of implant rehabilitations and to reduce the risk of complications during healing.
This is important in cases where implant restorations require a certain level of bone regeneration, as the predictability and stability of regenerated bone can play a major role in the success and survival of implant restorations: the type of implant surface/design and biomaterials used, various factors related to the surgery (submerged vs. non-submerged healing), to the prosthesis (abutment characteristics, platform change, etc.) and to the patient (systemic health, oral hygiene, compliance, etc.), may influence the expected results.
BIOLOGY OF BONE REGENERATION
From a biological point of view, a thorough understanding of the key steps and molecular events that take place during bone regeneration is of utmost importance to understand how different local and systemic factors can influence the regenerative process.
Based on the above, we could indicate that primary healing is a key aspect for the success of bone regenerative procedures. Clinician experience and manual dexterity, as well as patient compliance with pre- and post-operative instructions, are other key factors that can significantly influence the incidence of post-surgical complications.
When analysing clinical evidence, it is often difficult to isolate the effect of implant surface on implant outcomes and the stability of peri-implant bone regeneration, as implants differ not only in surface topography, but also in implant design, prosthetic connection and loading protocol.
To summarise, implant surface-related properties can have a significant impact and directly influence the regeneration of peri- implant bone defects. Therefore, proper adjustment of implant surface features is likely to further enhance bone regeneration in the future and could be a particularly valuable option when dealing with challenging clinical scenarios.
THE IMPACT OF PROSTHETIC FACTORS
Implant loading
Traditionally, dental implants have been prosthetically loaded after a healing phase of 3 to 6 months after stage I of implant surgery. However, in order to shorten the treatment time and to satisfy the requests of patients who are not willing to wait months before the restoration of edentulous areas (especially in the aesthetic zone), immediate and early prosthetic loading of implants has been introduced. At present, the different implant loading times are defined as follows:
- Immediate loading: when an implant-supported prosthesis is placed the same day or the day after implant placement.
- Early loading: when an implant-supported prosthesis is placed between 1 week and 2 months after implant placement.
- Conventional loading: when implants are allowed to heal for more than 2 months after implant placement without connecting a prosthesis.
Although immediate and early loading protocols offer the advantage of rapid rehabilitation, careful consideration of occlusion is recommended to minimise non-axial forces on the implant. In addition, adequate primary implant stability (30-35 N/cm) is a prerequisite for immediate loading, which can sometimes be difficult to achieve in the upper maxilla, where the bone tends to be more porous, as well as in patients with alveolar bone resorption requiring simultaneous bone regeneration along with implant placement.
THE IMPACT OF PATIENT-RELATED FACTORS
Treatment outcomes can be affected by multiple patient-related factors: gender, general health status, periodontal status, upper or lower jaw, as well as age at the time of implant placement are risk factors for implant loss.
It is therefore recommended to apply a patient-centred peri-implant care protocol with the following components for the prevention and treatment of diseases:
- Update of medical, social and oral history, risk assessment and patient feedback.
- Assessment of the oral situation: the health of peri-implant tissues, prosthetic components and the patient's ability to perform oral hygiene.
- Reinforce control of risk factors (e.g. smoking, dry mouth, glycaemic control).
- Professional intervention through an individualised oral health plan, including oral hygiene training and dentition/implant prophylaxis.
- Determination of check-up intervals according to the risk factors of the patient, the implant and the restoration.

Systemic diseases
In addition to underlying medical conditions (e.g. severe cardiovascular disease or cancer) that may put patients at risk during surgery, regardless of the nature of the intervention, different diseases that have a direct/indirect impact on bone and soft tissue healing can potentially affect the results of implant restorations.
Osteoporosis
Although it remains controversial whether osteoporosis has a detrimental effect on the jawbone, it is associated with reduced bone quality and increased cortical porosity in the jaws. Therefore, it is suggested that osteoporotic bone should be considered equivalent to type IV and that clinicians may consider a longer healing period for implant osseointegration prior to prosthesis insertion in patients with osteoporosis.

Tobacco
It is well established that smoking has a detrimental effect on wound and bone healing due to its local and systemic action. In addition to thermal injury, many irritants, toxins and carcinogens present in cigarette smoke can also cause changes in intraoral pH.
Notably, smoking also has a deleterious effect on vascularisation as nicotine increases platelet adherence, which can lead to the formation of micro clots, and ultimately, ischaemia.

Diabetes mellitus
Diabetes mellitus has been associated with the development of a number of complications in the skeletal system collectively referred to as "diabetic bone disease" or "diabetic osteopathy".

In conclusion, although the patient-related factors described above are not considered an absolute contraindication for implant-associated bone regeneration procedures, it is clear that they may influence the overall success of the treatment and the risk of complications.
Therefore, patient selection, management of underlying medical conditions and associated risk factors and, whenever necessary, consultation with the patient's physician are recommended.



